The recognition race of flu vs. COVID is on. The clear reason is minimizing a flood of viral illnesses we cannot distinguish come the fall. Anything we can do to mitigate the influx of patients to higher risk care settings is a national priority, and vaccination will be step one on the to-do list. It is informative to see how Australia experienced fall and winter in reverse of us and how they handled their blitz.
Have a look at the figure below.
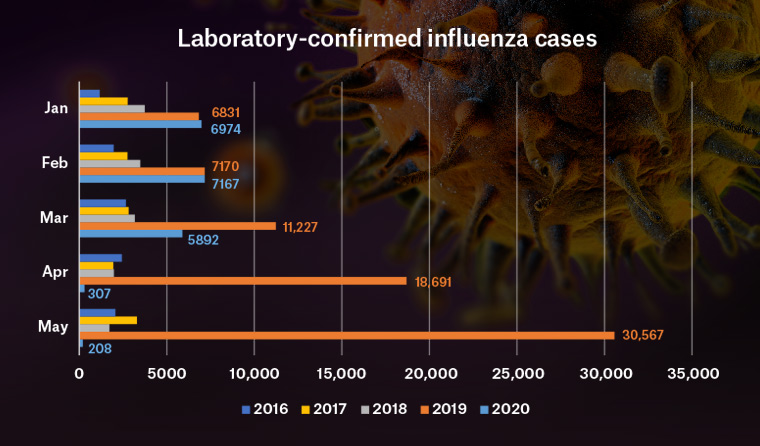
It’s safe to say the Aussies crushed it. But the massive reduction in cases they saw in April and May of this year was not due to the impact of the vaccine alone; it was also due to the spillover effects of masking and distancing secondary to corona. If the US adheres to the same degree as those down under, I expect we can see a similar outcome. In fact, I remember seeing some data earlier in the spring from the US, and what occurred here towards the tail end of our flu season paralleled the same trend.
Also of note, there were other reports of viral coinfections to the tune of 20% (mostly rhinovirus) in COVID positive patients throughout March. See HERE from JAMA. It’s the only study I have come across answering a question many of us will ask come cold and flu season: are we treating two problems and not one? In fact, we think the same way now with tick-borne diseases as coinfections are commonplace. Think viral panels.
Here, you will see a helpful review of the flu and coronavirus.
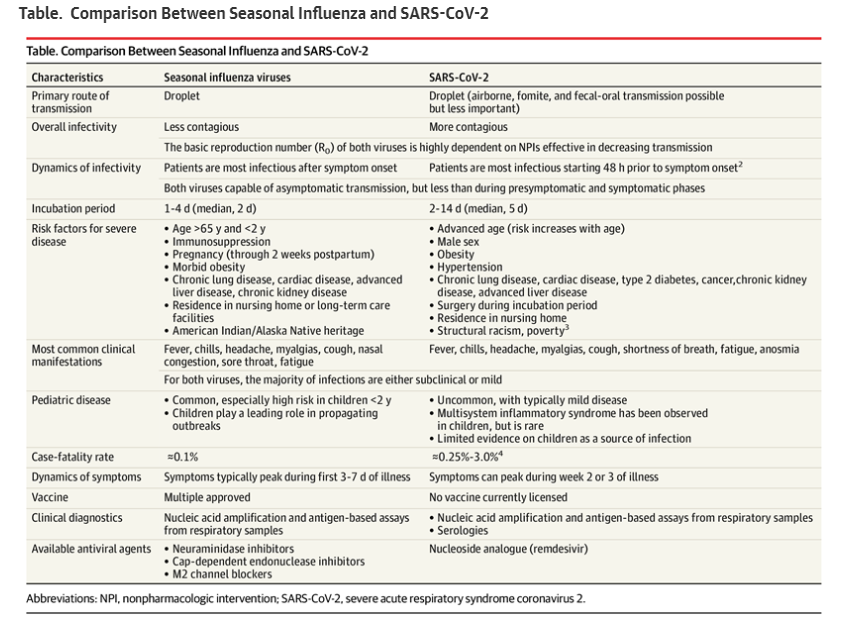
The discussion it comes from is HERE, and it’s quick and dirty. It’s worth taking a look at as other than school openings and COVID vaccine progress, prevention of respiratory illnesses like the flu will probably be the most frequent topic parked on our PC screen until after the holiday season.
PS: I’m telling my family to hold off on the flu vaccine until October. Remember, the maximum effect is 4-8 weeks after receiving it, and if past is prologue, peak flu season is December until March or so. While the shots may be available in a few weeks, it’s too early to get them. All bets are off if you have only one opportunity when you have face time with a patient, but availability and supply will be solid this year. With public campaigns, more patients than normal will be motivated to seek them out, so adherence should be better than average.



Flu is not acquired at all via fomites??? Also of note , the FLU seems to be much more seasonal but the COVID 19 seems to be year round…. UNLESS we see a drop in the Fall…. No, this is the first time I have posted….
The CDC’s recommendation on timing of flu vaccine is quite different than your comment above. DO NOT WAIT to receive flu vaccine. Patients should be vaccinated when possible out of concerns that a missed opportunity may result in failure to vaccinate at all.
The idea that flu shots should be delayed was phased out in the 90’s.
If the advice from CDC has changed, I would like to see it in writing.
Andrew
If its a one time opportunity, of course, give the shot–regardless of the time of year.
But maximum antibody protection from the shot is 1-2 months after administration. If you can delay until Oct 1, do so. This is good advice for seniors.
If you have recent evidence from trusted sources stating otherwise, please set me straight.
Brad
What about people getting a second flu shot, if they have already had themselves immunized? Thanks!
Dr. Flansbaum, antibody titer’s not a reliable indicator of protection against any viral infection following an immunization. The equally effective cell mediated repertoire defense mechanism but it’s not readily measurable. The CDC recommends getting the flu vaccine as soon as the vaccine becomes available and waiting is not recommended as there’s no proven best ideal time for vaccination
From the CDC website. Link within post:
“Vaccination too early in the season (e.g., July or August) may lead to suboptimal immunity later in the season, particularly among older adults.”