I am a skeptic of the physician evaluation component of HCAHPS. I suspect patients respond to hospital amenities, and better food, bigger TVs, and swankier lobbies have a halo effect—affecting how they assess not just the structural aspects of their care, but how they perceive their caregivers.
You probably share my bias. On an individual level, we can explain stellar assessments easily, because we all have a natural inclination to attribute good report cards to whatever brilliant skills we bring to the bedside. However, if we receive an appraisal mom would not want to pin to the refrigerator door, we activate our deflector shields and point towards the patient’s leaky sink, broken bed, and roommate with the earsplitting screams.
When our crosstown rivals reinforce those impressions by citing say, increased foot traffic post an upgrade (“build it and they will come“), we might be lulled into thinking designer labels win the day. Substitute some slippage in communication and care craft for a five star experience, and all will be well.
For those reasons, I vaulted into a recently released study entitled, Changes in patient satisfaction related to hospital renovation: Experience with a new clinical building. Johns Hopkins built a new hospital wing and they surveyed how the enhanced digs transformed their patient satisfaction measures. Here’s what the patients got:
Patients admitted to the new clinical building experienced several patient-centered design features. These features included easy access to healing gardens with a water feature, soaring lobbies, a collection of more than 500 works of art, well-decorated and light-filled patient rooms with sleeping accommodations for family members, sound-absorbing features in patient care corridors ranging from acoustical ceiling tiles to a quiet nurse-call system, and an interactive television network with Internet, movies, and games.
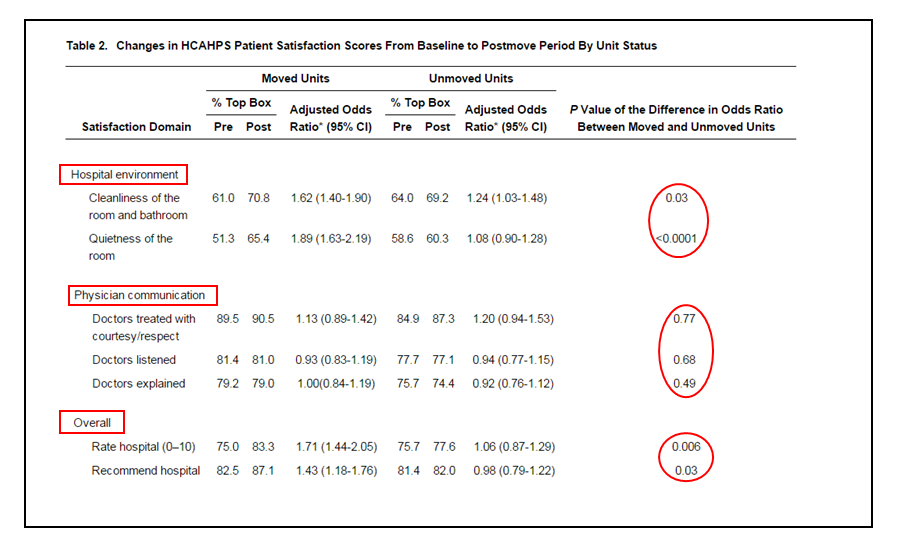
In essence, the buildings changed, but the caregiver teams didn’t. As a result, the investigators were able to compare pre and post HCAHPS and Press Ganey evaluations in a natural experiment—in both newer, upgraded units, and in older active ones.
What happened?
The findings surprised me. Not unexpectedly, the facility related assessments increased. However, the ratings for the staff remain unchanged, and the upgrades pre and post did not enhance patient perceptions of their docs. Non-facility ratings at the older wing also did not differ from the newer structure.
This is only one study, at one site, with a skewed patient population. However, we must be cautious; we may not like the findings and will find many reasons to dismiss the results. Like any good empiricist, I want to see further data with populations that are more heterogeneous and in varied locations. Nevertheless, for now, the Hopkins experiment serves as a good reminder that all caregivers should check their priors at the door. It just might be that what doctors do and say matters, and a first class meal and green gardens cannot paper over, or in the converse, sully our evaluations.


Hi Brad,
Thank you for discussing a very relevant article. As healthcare systems, administrators and providers work to improve HCAHPS evaluations (often with limited success), the article gives us insight into the impact of physical environment on patient satisfaction scores.
Though this is a single study, it appears that effect of hospital environment including features like noise reduction is limited, and human factors like better patient -provider communications need to be emphasized as means of improving patient satisfaction data.
Thanks.
Rupesh.
[…] the Hopkins study, Dr. Bradley Flansbaum, a physician at Lenox Hill Hospital, in Manhattan, wrote on the blog of the Society of Hospital Medicine that “it just might be that what doctors do and say matters, […]
[…] reading the Hopkins study, Dr. Bradley Flansbaum, a physician at Lenox Hill Hospital in Manhattan wrote on the blog of the Society of Hospital Medicine that “it just might be that what doctors do and say matters, […]
I had my first hospital stay in 60 years recently. The facility was old, but that did not matter. I got the surgeon I wanted and he was absolutely wonderful in every way, and the recovery room nurse was good also.
However, other than that, the stay was really dehumanizing. The ED doctor was poor (as opposed to the surgeon). I was dumped in a bed after surgery with a lot of monitors and ignored. The bell was answered and I was taken to the bathroom or whatever, but no one ever greeted me or asked how I was doing. When I asked about eating something 12 hours after my ended-at-midnight surgery, they didn’t bother checking with the surgeon who had said ice chips only immediately after surgery but said he’d be over sometime (which he was, several hours later) and could perhaps change the order then.
Yes, staff is far more important than the physical environment, though of course niceties are nice. I was desperate to get out of that place!
[…] reading the Hopkins study, Dr. Bradley Flansbaum, a physician at Lenox Hill Hospital in Manhattan wrote on the blog of the Society of Hospital Medicine that “it just might be that what doctors do and say […]
[…] most providers, The Hospital Leader is dismissive of patient experience scores, confident that patients only respond to big TVs, tasty […]