I am going to teach you something you do not know. I am almost sure of it.
Warm handoffs–a term you often hear within the confines of hospital walls when transferring a patient service to service or ward to ward. You do it in-house, but its unlikely you make the same connection when you discharge the same patient or transfer them to an outside entity.
But you have to be asleep under a rock not to have heard or read the changes afoot in the skilled nursing facility realm, including the rise of the SNFist. Too much variation in use and spending; plus, we are learning patients do not need twenty-five days couped up in a rehabilitation facility when fifteen might do with a segue into home health for another ten or fourteen. Patients like being home, and it costs a lot less.
Unfortunately, we do not do SNF handoffs in the same manner as ICUs. Our bad and inpatient providers better adopt.
As hospitals decant and quality measures get an intimate look in the rehab space, SNFs will notice sicker patients and the staff there will be more mindful of the signouts and the data they receive. Know a CMS value-based program starts on October 1 (just like hospitals–penalties and all) and SNFists, whoever they might be–NP/PA/DO/MD, will also require of hospitals a step up in information transfer–both in quality and timeliness.
MedPAC had a public hearing this month, and one of their presentations (short) had a persuasive slide you need to view:
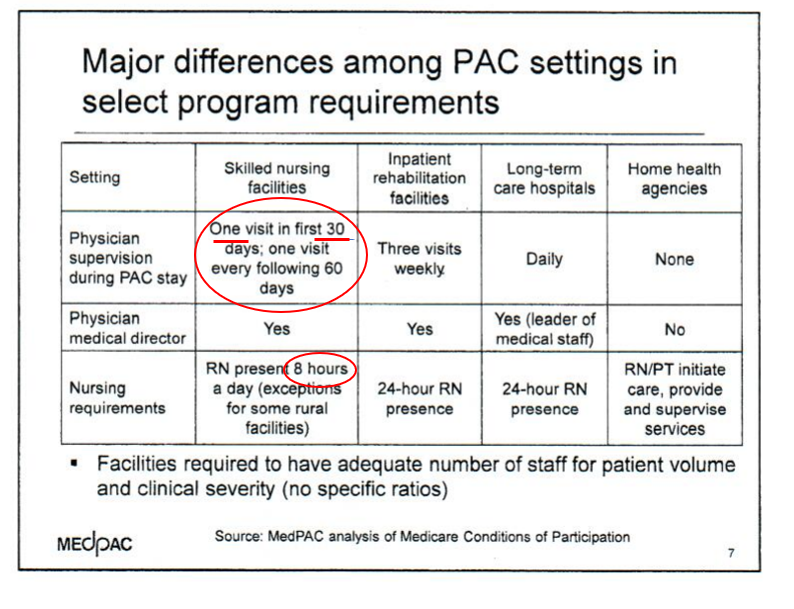
If you would not have noticed, I did the pleasure for you and highlighted the take homes.
–Did you know docs are not required to visit daily or even weekly?
–Did you know RNs are not a 24/7 presence?
I did not think so.
If the above is not a call to arms to tighten the sign out between the sites, let me give you more. A recent New York Times/Kaiser Health News report investigated staffing patterns at SNFs nationwide. In prior years, CMS relied on SNF self-reporting of staff to patient ratios (RN, LNP, CNA). Now, however, the auditing process is more precise, and the feds are using electronic payroll submissions for the star ratings folks see on the CMS site. You may be surprised to learn SNFs had woefully underreported weekends, overall RN presence, and CNA support in many facilities and hence, we can infer patient supervision was lacking. At best, patients usually get 3-4 hours of staff time daily. With the fresh facts, you can bet patients get a fraction of that in some outlier facilities. The story and data maps are 100% worth your time so scan the article to get up to speed. Congress also took notice, and they are asking CMS for more information and oversight on the matter.
So getting back to the warm handoffs. SNFs are getting sicker patients; staffing and supervision are lacking; on-site capabilities are varied and NOT equal to hospitals (not close); so SNFists, as they grow in numbers and begin to coalesce as a field, will require better reports and verbal connects.
In the era of shared risk, bundles, ACOs, and preferred SNF networks, leaders will call upon you to broaden your reach outside hospital walls. This is especially true knowing one of your collaborators will be five, ten, or fifteen miles down the road receiving your inpatient handiwork–with no desire to see it torpedoed with a bungled handoff containing false intel, or worse, incoherent chicken scratch.



About those hospitals…..
Are you familiar with the term “discharge to cab?”
I thought it was myth until a hospital almost did it to my mother (I’m a health care admin geek and my wife is the best (retired) geriatric nurse on the planet, and we rearranged the thinking in the emergency department in shsort order). Then we saw it again at a different hospital ED.
Hospitalists, health thyself.