You have read constant references about ACOs (accountable care organizations) in every journal you pick up until you are blue in the face, I’m sure. You or your hospital might even be participating in one.
Mostly all straight Medicare patients (the two-thirds not in Managed Medicare) are eligible for inclusion. You need two things to be in the ACO fiesta: 1) to live in an area where a health system has worked with CMS to set up an ACO, and 2) have most of your care as a patient attributed to a provider participating in that system. Patients don’t sign up, and CMS doesn’t ask docs for permission. Uncle Sam AUTOMATICALLY assigns folks to a hospital system’s panel. Them’s the rules.
Now here is why today’s post is essential reading. Pay attention.
Put aside the fact healthcare utilization is over the top and everyone plus their grandmother wants to rein it in. Being in an ACO doubles down on that spending gone wild and puts any participating accountable care outfit at risk for losses (or gains) their member patients incur at any place at any time. We, hospital-based providers, hold super-sized keys to the spending kingdom for any participating ACO patients.
In other words. CMS looks at the TOTAL spend for a Medicare member over a year–regardless of whether the patient utilizes services within their “assigned ACO system” or not, in this case,, again, [INSERT YOUR ACO HERE].
You will see why you have to watch everything you do as a result of being participants. See below as one possible illustrative example of a random CMS risk track your hospital or system could enter into. It is a two-sided risk model–the soon to be standard for all participants after 2-3 years of signing a CMS contract to play ball.
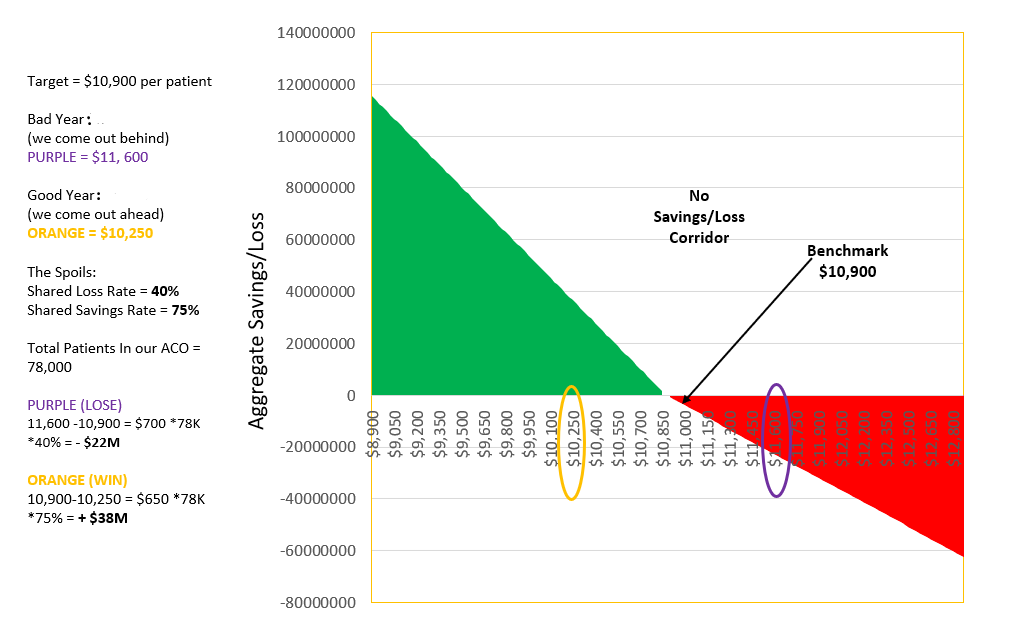
In the example above a Medicare patient, on average, will use $10,900 of services per annum (as context, a 30s yo adult with typical use in a year might incur $1-2K of spend).
View the math above. Come under our assigned spend benchmark, in this case at $10,250, and your ACO wins. Conversely, blow through the cap at $11,600, and you lose.
You can see a lot is at stake. You do not need a degree from MIT to add up the manna.
Now, do you see why the ACO has salience to what we do? Leakage to systems other than yours, post-acute care…stuff we don’t provide under the normal hospital roof. Any system-based ACO is accountable for ALL of it, and the cost accrues into its bucket, so it behooves any doc in a hospital who touches or has an impact on a participating patient to manage and track care wisely.
Got it, now?
As an aside, the consolidation that results to keep an integrated system’s patient base contained can help a system as much as it can wreak havoc on health care prices in the region it sits in. Monopoly power–a potentially unwarranted adverse consequence of ACOs–is getting more and more attention. See here. All that glitters may not always be gold.



Leave A Comment