JAMA just published the largest trial I have seen on a Hospital at Home (HAH) model to date and the first one out in the last few years. It comes from Mount Sinai in NYC–who have led the pack in this style of care if national presentations are the judge.
They launched the program three years ago on a grant—and financial feasibility, once pilots like these get pulled from their funding lifelines, is the whole nut. Essential to keep in mind. They cared for about 300 Medicare patients and dedicated staff and equipment to manage 19 different diagnoses in the home setting. Folks came from referrals in doc’s offices or directly from the ED.
It is important to note, this was NOT an RCT and the comparator group, younger and less sick, which presumably would bias the results towards the controls, came from a pool of patients who presented when screening was unavailable (4P to 8A and weekends). Investigators made the appropriate variable adjustments.
Patients were not eligible if home safety could not be assured and they had clinical factors making them too risky (arrhythmias, clinical instability). Obvious stuff. The flow diagram in the paper nicely illustrates who got registered and the reasons for their study refusal or dismissal.
As an aside, Australian (HaH is standard of care there) and smaller but similar US programs enroll up to approximately 5% of individuals who normally might be inpatients. Based on their outcomes, if if done right, 90% or so will stay put at home and recover without a need to hit the ER. Financial feasibility to support a team of staff is likely 200 or so patients per year (~4/week).
Translation: 5% of hospital beds could be vacant if this is our future. Given hospital occupancy trends are down trending–US average in the 60s percent range–and have been for a decade plus, that’s a big whack.
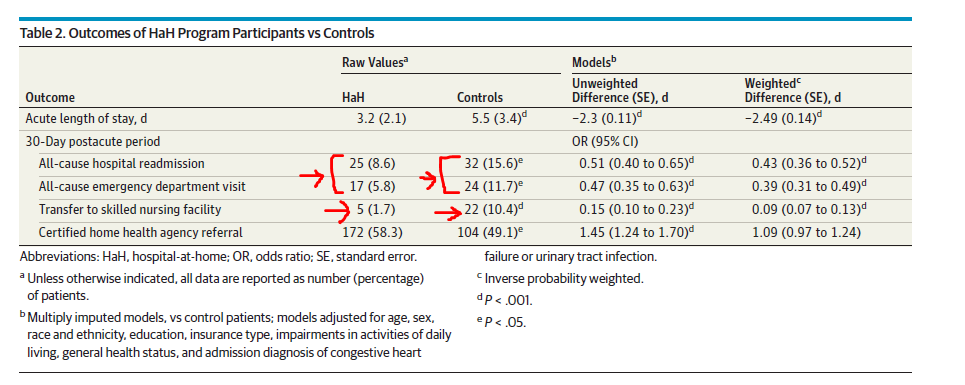
To cut to the chase, the investigators measured the usual outcomes of interest and patient satisfaction. The “LOS” for HaH patients is the start time staff provided hospital-level care to them in their home (or apartment, more than likely). Here is the manna:
OUTCOMES:
HCAHPS:
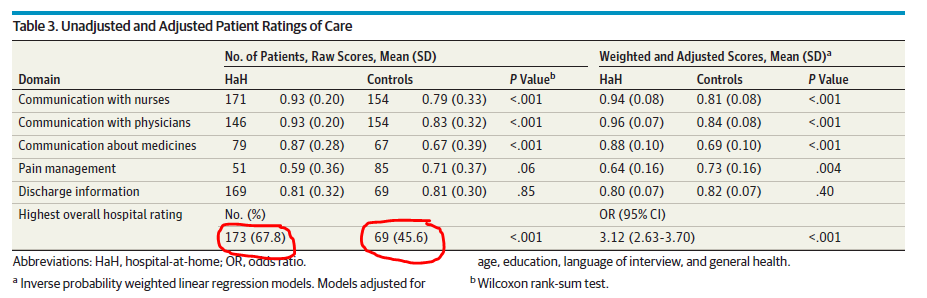
Bear in mind, again, this is an observational trial with selected patients. However, the results still raise eyebrows; patients do well at home and are happier there If providers screen them right.
The next step will be designing a payment model everyone can work with—payers and providers alike. The Sinai folks have proposed a 30-day bundle for CMS to review to cover the full acute and post-transition 30 days of care. CMS will have to analyze the scheme closely as the bundle could be gamed by flipping patients too easily into a HaH setting when outpatient management might do. As always, substitution effects and unsavory behavior are omnipresent. What else is new.
Will this be the future of health systems, to the detriment of acute care facilities? Most definitely. Urban versus rural settings will make a difference in pace of adoption, but workarounds for settings will not be the rate-limiting step. It will be all about payment and financial feasibility. That’s the 800-pound gorilla. But yes, it means more vacated inpatient beds and less need for inpatient providers in the coming years. That’s why I am highlighting the study here. There is an editorial to the piece as well and the discussants point out other important issues to take note of.



Nice summary!
Could this be an opportunity for hospitalist telemedicine. Imagine rounding on say 15 at home patients a day.