“We Need Creative Solutions”
When I read or hear the sentence above, I think of one thing and one thing only. The solution is long in coming, involves input from multiple parties, has no obvious fix, is costly–in either money or time, and we undergird it by a whopper of a collective action problem.
How about getting to the actual point:
“The problem we are trying to solve has no answer. We likely know the best course, and it’s staring us in the face. We can spend the next few days, weeks, or months pretending we are unaware of it or we can take half a loaf now and get back to work.”
The above ran through my mind as I read a new hospital transitions study out in Annals of Internal Medicine. The findings were not unexpected, by me at least, but the response by those who do not deal with the issue firsthand will read it and by way of the “creative solutions” contrivance above assume there is a simple answer. Hospital and post-acute facility blame will be sure to follow. Teams of providers will sit around a table, and point fingers engaged a round-robin blame game that should not have to be.
Back to the paper.
The study retrospectively culled Medicare patients between 2006-11 whose death occurred 30 and 90 days after a post-acute care facility stay. Eight million beneficiaries died in total during that five-year period, and of those, two million had a PAC visit within 90 days of their death (25%).
What caught my eye and interested me most, was the number of seniors admitted back to the hospital within 90-days (again, by way of PACs). A staggering 60% or 1.2M individuals returned to the hospital. See the table below:
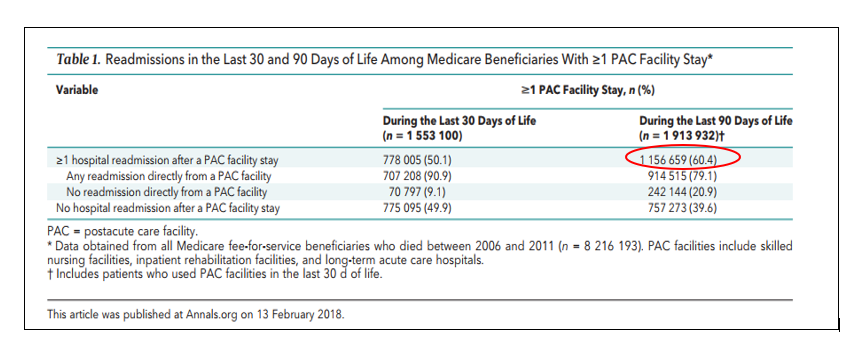
Keep in mind; the study analyzed decedents–folks the investigators knew who died–so this is a morbid cohort by definition. An ill patient will cycle from acute to post-acute to home and back because caregivers cannot predict an imminent death with precision (“do everything until you can’t”).
But that 1.2M number looms large, and it does not stem from the failure of providers to read the prognostic tea leaves. They know the appropriate time for hospice or intensive palliative care in many elderly infirmed patients.
People, when asked about where they wish to spend their last days, will express a desire to be at home with family, and the institutional revolving door is not what they want. Why in the heck then, are people spinning through them in a pointless circuit.
The go-to, ready at hand answer is failure to huddle the parties involved so they can talk and coordinate. If hospitals, ERs, and PACs just communicated the problem would vanish, and we all could move on to the next healthcare dysfunction dumpster fire.
For those who know better, however, the above view roots itself not from a page out of Deming’s playbook, but in behaviors hardwired into our coding and billing system, and an inadequate community safety net unable to meet the needs all parties involved demand.
This is reality:
a) We communicate with an ill patient or their family. We express the patient has little chance of benefitting from inpatient rehabilitation.
b) However, we present the above option with caveats and recommend against a SNF, with its false hope and attendant risks. We transition the discussion into hospice.
c) The patient or family opt for home hospice. Facility representatives discuss options.
d) Home hospice does not provide 24/7 supervision. All the family works and is out of the house during the day. Forget home hospice.
e) Inpatient hospice pursued. The patient will likely require several weeks of support as their life expectancy is greater than a month.
But the figure below will clue you as to what happens next:
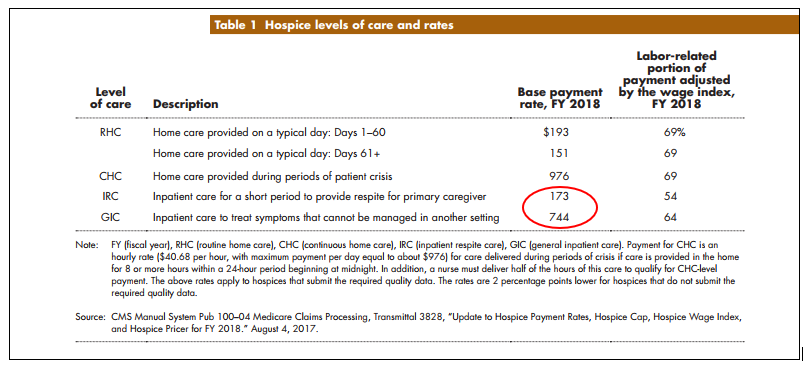
Note there is no long-term rate for conventional inpatient hospice and the options for home, again, hinge on available family or friends. The patient then, as if an oracle flips a switch, “becomes a reasonable rehab candidate” (with reimbursement of ~$400/day) along with an express lane ticket back and forth to the ER and hospital for rescue care.
SNFs understandably, do not manage severe shortness of breath, abdominal pain, and fevers of 102ºF. While some facilities go above and beyond and provide the palliative care and nurturing dying patients require, they are not hospitals or hospice units. In the majority of cases, things do not work out as planned. Off-hour skilled nursing facility shift personnel are not equipped to handle panicked patients and families, and they do what any rational person would do. Call 911.
Wrong care, wrong time, wrong place.
ER docs, intensivists, and hospitalists render the treatments on return to the hospital because folks residing in SNFs deserve and “require” it–or else why would they be there in the first place. Again, judicious management.
Creative solutions mean community resources to keep dying patients at home and safe. It means aides, expertise, access to professionals and confidence in the house–all of which are in short supply or nonexistent. And if the home environment cannot provide what patients need, we require a skilled locale to turn to whose purpose supports what hospitals and ERs inappropriately engage in now–unwelcome acute care.
So, it’s hospital > SNF > ER > hospital > SNF and more results like in the study above until the system rights itself and we, to phrase in a secular manner, have our come to Jesus moment.
What a woeful waste. Solutions of this sort require a suite of payment and regulatory fixes from Congress and CMS. We, the humble providers, can tinker around the edges because that is all we can do. It’s taking that half a loaf. More advanced directives, more attempts at home hospice, and more mutual “signaling” between PAC sites and the hospital is all we got.
But with the wins will come losses with unnecessary human suffering. The care variations we see around the country where some regions might be doing it better—with the implied message of facility underperformance—likely has more to do with local resources on hand than what facilities fail to implement. Applying the half fixes require a degree of risk and uncertainty people should not have to bear.



Great post!
[…] Hospital Leader (not to be confused with the Dear Leader) helpfully explains that “We need creative […]
[…] Hospital Leader (not to be confused with the Dear Leader) helpfully explains that “We need creative […]
[…] Hospital Leader (not to be confused with the Dear Leader) helpfully explains that “We need creative […]
[…] Hospital Leader (not to be confused with the Dear Leader) helpfully explains that “We need creative […]
Medicare will pay either for acute rehabilitation or hospice. There is nothing in-between. Hospitals want to reduce in-house mortality and reduce 30 day re-admits. They are strongly incentivized to push patients into hospice. Families elect hospice after being tempted by more in-home support. Hospices must persuade CMS they are taking only patients with < 6 month life expectancies, and are sanctioned if too many of their patients live longer than 6 months. They are highly incentivized by a per diem payment model to minimize expenditures on patients. Once in hospice, elders are persuaded against obtaining acute care, even for easily reversible problems. Who is speaking on behalf of frail elders who simply need good, in-home maintenance care to live out the rest of their lives in dignity?