The COVID-19 pandemic has changed health care as we know it. It has sowed fear and doubt among the public and created endless questions without answers. Our hospitalized patients may wonder why they can’t have their families beside them and worry about contracting the virus in the hospital. Strict visitation policies only add to their fear and anxiety.
Given these challenges, authentic connections between hospitalists, patients, and families are more critical now than ever. But how do we even begin to build rapport while wearing impersonal PPE gowns and N-95 masks? The answer: we need to go the extra mile to win our patients’ trust and confidence.
Early in the pandemic, I frequently found myself experiencing profound challenges that I’d never faced before. How do I communicate the ever-changing CDC recommendations around COVID-19 management to my teams? How can I comfort patients who feared they’d never see their loved ones again? I could see the look of uncertainty and fear in the eyes of my fellow providers and could understand the anger and loss from those family members were suddenly quarantined with no warning. Throughout those turbulent months, I wished hospitalists had a playbook to help us navigate these emotionally-charged situations.
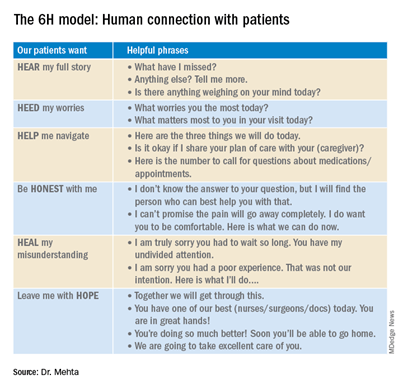
To this end, I shared a framework called the 6H Model of Connection in August 2020 issue of The Hospitalist. However, as the pandemic ground on, I felt physicians needed even more support to close the communication gap. I reached out to my peers at SHM’s Patient Experience Special Interest Group and realized we all were facing this same problem. Together, we created some brief but impactful scripting for hospitalists facing five tough pandemic-era situations.
Patients with COVID-19 who are fearful of their clinical prognosis
The impact, medical management, and long-term prognosis of COVID-19 is a source of concern and fear for most COVID-19 patients. Here’s some scripting based on the 6H model to guide these conversations:
Hear and Heed:
- “What have you been thinking about COVID and how it impacts you?”
- “What worries you most today?”
- “Is there anything you want us to know if your disease gets really bad?”
Help Navigate:
- “Our team is here for you and prepared to care for you at every step.”
- “Here are the three things we will do today to keep you safe and help you get better.”
Be Honest:
- “It’s normal to be a little scared. Today, we will be doing XYZ, and we hope you will recover. Our team is here for you.”
- “We might not know everything about this disease yet, but here is what we are doing to protect you and ensure you get better quickly.”
Helping patients and families cope with visitor restrictions
Being hospitalized is one of the scariest experiences we can endure. It’s natural to want our loved ones at the bedside comforting and advocating for us — and our families want to be there too. So it’s no surprise that visitor restrictions often spark angry outbursts, even if these rules are intended to save lives. We can soothe frustrations by addressing the “why” behind our policies and emphasizing other ways clinicians, patients, and families can communicate. Here’s how we might use the 6H Model to guide these delicate conversations.
Hear and Heed:
- “What worries you most today?”
- “Is there anything else we can be doing during this difficult time?”
Help Navigate:
- “Dr. X, the oncoming hospitalist, will update your family on your progress at [the family’s] preferred time.”
Heal Communication Gap:
- “I apologize. We can’t allow visitors at this time. I can see how it seems unfair. These are rules for ALL our patients in order to keep everyone safe. We will make sure to keep you and your loved ones involved and updated.”
- “Thank you for your patience and understanding as we navigate this pandemic and take precautions to keep XYZ hospital safe for all our patients and staff.”
Overcoming communication barriers caused by PPE
More than 70% of communication is nonverbal. Anxious patients and families constantly scan our faces and bodies for unspoken messages. So, it’s no surprise that masks and gowns create barriers to rapport and trust. Lack of physical contact like handshakes and reassuring touch only adds to the disconnect. Here are some ways we can compensate:
Consider displaying your name and photo on a whiteboard in the patient’s room and on a badge on your gown. Make good eye contact, speak clearly and slowly, lean in, and nod to show understanding.
Hear & Heed:
- Listen, summarize, and ask clarifying questions. “I want to make sure I’ve got everything. What have I missed?”
Human Connection:
- “Tell me one thing about yourself, like your favorite hobby/sports team/food.”
- “I wish we could see each other’s faces today. Please excuse my astronaut gear. I apologize for the inconvenience. I really want to know what’s on your mind today.”
Soothing the loneliness and isolation all patients experience during this pandemic
COVID-19 is a terribly lonely disease that has highlighted the depression and helplessness our elderly patients often feel. Patients look to us not only to treat their disease but also to provide connection and reassurance during their hospital stay. Here are some phrases I’ve found helpful when addressing this very tender problem.
Hear & Heed:
- “I realize this experience can make you feel alone in the hospital. What worries you most?”
Help Navigate:
- “It must be hard to be in the hospital alone. We are here for you.”
- “Is there a friend or family or clergy member with whom I can arrange a virtual visit for you?”
- “Here is how you can call your loved ones any time and see and hear them.”
Be Honest:
- “These are tough times. I would feel the same way if I were hospitalized right now. I want you to know I’m here for you.”
Hope:
- “I’m optimistic you will soon see your friends and family in person.”; “We will fight this disease together and overcome it.”
Reassuring patients who are afraid of catching COVID-19 in the hospital
During rounding, I encountered many patients admitted for diabetic complications, sepsis, and heart failure who worried about catching the virus during their stay. Some patients won’t voice their concerns unless we invite them to share. This gives us an opportunity to provide expert reassurance and comfort.
Hear & Heed:
- “Tell me more… what worries you the most?”
Help Navigate:
- “I want to reassure you we are taking the strictest precautions and measures to keep you safe. [Mention specific measures like sanitizing surfaces, PPE, visitor temperature checks, etc.]”
Hope:
- “I realize this is a very scary time. I’m confident we will get through this and get you home to your family soon.”
- “These are extraordinary times, and we’ll overcome this together.”
Patients with vaccine questions and concerns
A new conundrum for hospitalists involves the COVID-19 vaccine. Is it safe? When can we get it? Which brand is best? Does it work?
I can also see unspoken questions in my patients’ eyes. Why didn’t I receive it yet, doc? Is it because of my of skin color? My zip code? Why should I trust a healthcare system that has exploited my community in the past?
The responsibility of fostering trust in the vaccine and delivery process shouldn’t lie solely with the government. As health care providers, we are in well-positioned to correct misinformation and bolster patients’ vaccine confidence. It’s important that patients understand not only why they need to get vaccinated but how. Here are some tips:
Hear & Heed:
- “Tell me more about your worries and doubts. I want to know.”
Help Navigate:
- “Here are the current vaccine guidelines. I also have a list of places where you can get vaccinated.” [Have up-to-date handouts you can distribute.]
Be Honest & Give Hope:
- “I can only imagine how confusing this has been. There’s so much conflicting information coming at you from different sources. I want to reassure you that the vaccine is safe and will protect you. I did a thorough review of the evidence behind the vaccines. I took the vaccine as soon as I could in order to keep my patients, my family and myself safe.”
If they are not eligible yet based on state guidelines: “How I wish we could speed things up. Your health is our top priority, and as soon as you are eligible, I urge you to sign up and receive the vaccine.”
No one has felt the “wartime conditions” created by the pandemic more than healthcare workers. Hospitalists are among the brave warriors who must tend to the wounded, weary, lonely, and disheartened and heal their souls along with their physical wounds. Just as medicine is salve to the body, information and attention will nourish hearts and minds. Leveraging the 6H Model, I believe we can convey compassion, gain patients’ trust, and truly connect with them at this crucial time.



Excellent, I really enjoyed reading.