A few years ago, I visited Mt. St. Helens and was astonished by nature’s power. After the volcano erupted, the summit vanished, and the mountain around it was destroyed under a thick blanket of ash. Now, it felt like the world around me had again changed just as quickly, but invisibly and with a more cruel and devastating impact.
The text message arrived at 8:07 p.m. on February 28: “Coronavirus positive. Call me.”
I could almost feel my heart stop. A patient of mine in the ICU, admitted from a nearby nursing home, had developed worsening respiratory failure that week, without a clear etiology, and tested positive for SARS-CoV2 as soon as CDC testing guidance changed. Suddenly, the world transformed: I was put in quarantine, unable to see my teenage boys, unable to support my colleagues on the front lines. My patient passed away. As I paced the house, afraid of developing a fever and respiratory failure myself, phone calls and emails flooded in. Monthly work meetings became daily meetings, where we discussed constantly changing CDC and DOH guidelines, PPE and testing, isolation of patients, discharge guidelines, the no-visitor policy and anything else that happened to come up that day.
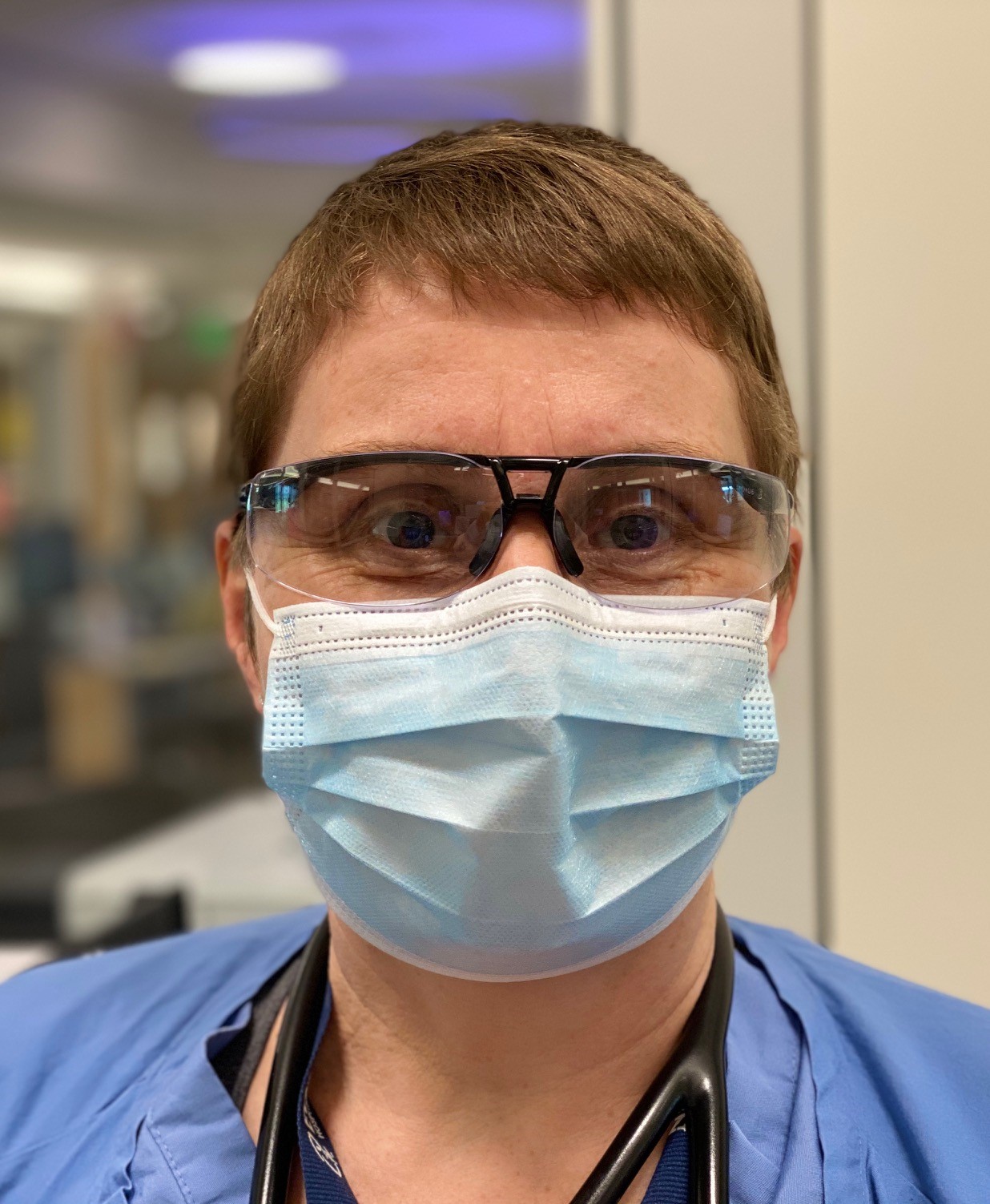
After ten days in quarantine, I hardly recognized our hospital anymore. Gone was the steady flow of traffic through the hospital hallways, with patients being admitted for strokes, heart attacks and scheduled surgeries. Instead, we only heard muffled voices from hospital staff communicating through N95s, goggles and face masks, avoiding any closeness. Smiles were replaced by serious and concerned looks.
In those starkest, earliest days of the pandemic, Shirley and Bob* came to the hospital from their assisted living facility, both positive for COVID-19. They had been married 52 years. Shirley was a young nursing student when she met Bob who worked as a carpenter. They had two children and five grandchildren. Shirley’s eyes lit up when she talked about Bob and the adventures they had together; then, she would melt in tears as she spoke about his death. I attempted to console her, desperately trying to find the right words. She did a better job than I did, expressing her gratitude that being infected with coronavirus allowed her to be with Bob during his last hours. Had she tested negative, she wouldn’t have been allowed to be with him when he passed away. How humbling, her words – and her attitude.
Tigger and Eeyore – the nicknames of another COVID-positive couple – had been living in a memory care unit. Tigger was feisty, suffering from dementia. Her husband, Eeyore, previously had a stroke and now could hardly speak; we expected him to decease quickly. Tigger said Eeyore loved his stuffed donkey (of the same name, of course), but there was no one to bring the donkey from their home. By chance, a colleague’s stuffed donkey looked almost like the real Eeyore, and the patient passed away peacefully with a stuffed Eeyore in his arms and his real Tigger at his side. In the aftermath, Tigger occasionally forgot that her husband had passed, but you could feel her deep love for him when she hugged her stuffed Eeyore tightly.
The pandemic has transformed me into a social worker, chaplain and a distant family member in addition to my physician role. My days now are focused on providing more emotional than physical support to patients and their loved ones. Patients aren’t the only ones that need emotional support. Nurses, RTs, OT/PTs and all the support staff feel unmoored during this crisis as well. Since COVID-19, our floor nurses have witnessed more deaths on a daily basis and in a crueler way. Isolated, gowned, goggled, gloved and masked, they provide end-of-life care without being able to hold their patient’s hand to say goodbye. One of our cheeriest nurses who always cracked jokes has eyes filled with tears regularly as another of her patients passes; I can’t help but hug and cry with her.
Not all has been tears and death. Some patients overcome this unpredictable virus after a valiant fight, and some barely seem touched by it. Paul, the 47-year-old father of a 10-year-old son, was intubated in the ICU for almost 14 days, extremely sick and weak. After a four-week hospital stay, I was able to discharge him home. Sue, a 95-year-old lady admitted after a fall at her assisted living facility, was only tested because of the pandemic and didn’t cough once.
Our society is now a few months into this crisis. Life has changed for all of us. We are slowly getting adjusted to this new world of universal masking and social distancing. It is too early to envision how the future will look for us as healthcare workers – or for my two sons and their friends who are becoming young adults.
May 2020 marked the 40th anniversary of Mt. St. Helens’ eruption. Although everything appeared to be lifeless and destroyed after this natural disaster, deep under the ground, there was life. Slowly, new plants were able to bloom again, like the purple-blue wildflower, prairie lupine, with the help of the pocket gopher. I vividly remember how colorful they were in contrast to the desert-like surroundings after the blast.
Full of hope, I strongly believe that with time, we all also will rise from the ashes, recover from this pandemic and see the beautiful side of healthcare and the world again. There are seeds of hope everywhere, waiting to bloom.
*AUTHOR’S NOTE:
This is a fictionalized account of true events that I encountered at my hospital, EvergreenHealth, in Kirkland, WA. I, the author, have changed names and exact details to my discretion.


So beautiful…
Thank you!
Your hospital was so hard hit. Thank you for sharing so wonderfully.
Thank you!
Thank you so much for providing inspiration and hope! Hospital Medicine needs physicians like you, now more than ever. Danielle Scheurer
Thanks so much Danielle
Very insightful thank you for your courageous work!
Thank you for providing insight into the early days of COVID unfolding. Such profound effects. May you find light ahead.
Thanks so much. Stay safe. From a Hospice Care Center RN
This is so beautiful Angelika.
Angelika, I so enjoyed your article. You presented the human side of Covid, and that is a crucial component. Yes, you became a social worker, chaplain, and distant relative for these suffering patients, their families, and the staff. I’m thankful that you were there for them and that you did not develop the virus yourself. I miss you and the other doctors at Evergreen.