Mark Smith, MD, MBA, was the founding CEO of the California HealthCare Foundation; he served in that role for 17 years before stepping down last year. I’ve known Mark since we were residents together at UCSF in the mid-1980s, and both of us were influenced by training at the epicenter of the AIDS epidemic. Mark continues to see AIDS patients at San Francisco General Hospital one day each week. He was the lead author of Best Care at Lower Cost, a major Institute of Medicine report, published in 2012. Mark is one of those rare people who can take complex and politically charged concepts and distill them into sensible nuggets – while managing to be hilarious and profound at the same time.
In the continuing series of interviews I conducted for my upcoming book, The Digital Doctor: Hope, Hype, and Harm at the Dawn of Medicine’s Computer Age, here are excerpts of my interview with Mark Smith, conducted on July 24, 2014.
Bob Wachter: Put yourself back about 10 or 15 years ago when you were thinking about the promise of healthcare IT. As you’ve watched the last 15 years play out, what’s been surprising to you?
 Mark Smith: As with most of life, it’s a lot harder in fact than in theory. My first hint of this came with the implementation of computerized order entry at Cedars-Sinai in 2002. [In a story I tell in the book, Cedars’ physicians all but threatened to go on strike after they turned on the clunky system. Within a month, they pulled the plug on the system, a hiccup that cost the organization $34 million in 2002 dollars.] That was my first window into the gap between what sounds lovely in a policy paper, and what it means in practice to implement this stuff.
Mark Smith: As with most of life, it’s a lot harder in fact than in theory. My first hint of this came with the implementation of computerized order entry at Cedars-Sinai in 2002. [In a story I tell in the book, Cedars’ physicians all but threatened to go on strike after they turned on the clunky system. Within a month, they pulled the plug on the system, a hiccup that cost the organization $34 million in 2002 dollars.] That was my first window into the gap between what sounds lovely in a policy paper, and what it means in practice to implement this stuff.
Some of the issue is generational. As it turns out, a lot of other things that older doctors find troubling and resist – such as protocol-based care and quality reporting – track nicely with the tools through which they are supposed to do these things, namely IT.
When I talk to groups of docs, I always start by saying there are at least three groups of you here. There are younger docs who find all this stuff completely rational – it’s part of your vision of medicine. There are older docs who, depending on the state of your Roth IRA, are basically done. You’re not going to change a lot, and when you are finally forced to… fuck it, you’re done.
Then there’s a fairly big group in the middle that is caught between their expectations and the reality. That is where the grumpiest and the most scared people are. That is the group we’ve got to concentrate on. My sense is trying to get every single doc to use the technology or to feel comfortable with it is a lost cause. They will eventually retire, move off the stage, or be in practices that will eventually wither and die.
BW: I wonder whether that middle group is angry at technology because it has invaded their space. There it is, and you can pound it with your fist. It’s easier to be pissed off at your computer than at the National Quality Forum, Medicare, the Joint Commission, etc.
MS: Yes. It’s a little more visible and a little more understandable for people. If you’re a practicing doc, the RUC and Meaningful Use and the SGR – these are abstractions. But when someone says the ergonomics of your everyday practice are going to change in the following way, that becomes the focal point for a lot of your anger and resistance.
BW: Do you have any theories as to why, in this industry that represents one-sixth of our economy, the information technology systems are so bad?
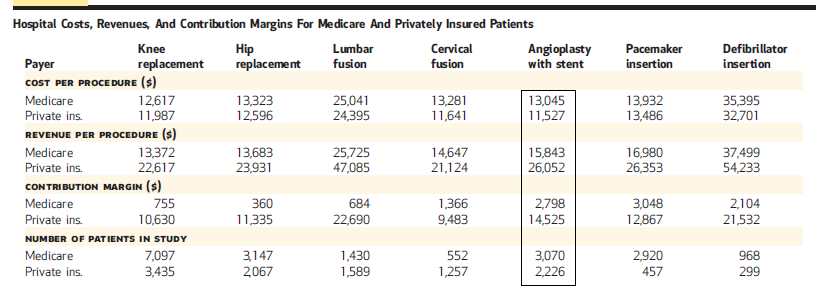
MS: I think a lot of it is in the economics. In healthcare, the reimbursement policies are at best neutral and often are inimical to IT adoption. There’s a wonderful article on the adoption of EMRs in Hawaii, at Kaiser. It turns out they had a lovely before-and-after natural experiment. When they implemented their EMR, patient satisfaction went up; provider satisfaction went up; quality measures went up; visits dropped by 27%. Now, at Kaiser that’s a good thing. But for most of American medicine, that’s an economic disaster. To the extent that the world is still largely driven by volume, and one of the first effects of consumer-oriented IT is to decrease the volume of traditional visits – well, it’s no secret why that doesn’t happen naturally.
The second is that if you think about a company’s motivation to make easier, more intuitive, more beautiful IT for your phone, it’s because if they put it out there, people will gravitate to it and they will make a bunch of money. That’s not the way the IT in healthcare gets adopted or sold. It’s largely one corporate executive selling to another corporate executive, and the docs and the nurses have no say. The instant market gratification of putting out something that people really like, something that’s easy to use – that feedback loop doesn’t exist, because health IT is still largely a B2B [business to business] phenomenon.
BW: If you were in Washington in 2008 and somebody gave you $30 billion to spend on health IT, would you have spent it the way the government did?
MS: My sense is that they missed an opportunity to impose or to bring about standards, which would have let the IT people compete on the interface. In other words, if the backbone of the data were standardized, then you could have IT companies not competing on standards, but competing on the beauty of their interface, the intuitiveness of their interaction with providers. What we have instead is competition all up and down the vertical, and that I think is the tragedy.
That’s the magic of HTML, right? Most people have Windows, some people have Macs, some people have Linux – you can choose whatever interface you like. Companies compete on the intuitiveness, the attractiveness, and the beauty of the interface. Whoever does that well will win.
Smith’s California HealthCare Foundation was the major funder, to the tune of $10 million, of one of the first efforts to build a regional health information exchange, in Santa Barbara, California. After a few years, it failed. I asked him to reflect on that experience.
MS: The central lesson was that, despite all the rhetoric about what happens if your patient was in an emergency room across town, there was no convincing business model about why people should spend private money for this public place.
The reality then, and I believe now, is that if your objective is to improve care, that has much more to do with improving communication within the clinical ecology in which most patients get most of their care than with having some universal communication between ecologies.
At a recent talk, somebody asked me, “Well what if the patient is in an ER across town?” I said, when I was a resident, if they were in an ER across town, you picked up the damn phone and called them.
It’s not that that a robust information exchange wouldn’t be a good thing, but, given what it takes to create that kind of public good compared to how often that happens and its impact on day-to-day quality of care – it just wouldn’t be my first priority.
But that was then, this is now. Part of what’s happening is that those docs who were semi-independent 10 years ago are now in an ACO or have been bought. With consolidation comes a greater opportunity for a unitary system, within an ecology. These ecologies are getting better and better, and more and more sharply defined all the time.
The other thing is, the technology’s a lot better. At the time you didn’t have the easy possibility of data sharing and interchangeability without people actually all giving their data to one big database. Now you do.
We turned to the question of patient portals. I asked Smith how important patient access to their own data is, and where he sees this area heading. Both of us were on the Google Health advisory board, an effort by the company to create an early consumer-facing healthcare portal. It failed miserably, and Google pulled the plug on it in 2012. He began by discussing another corporate effort to provide data to patients.
MS: I was also on the Qualcomm Life Advisory Committee. Of course, they’re pushing to allow everybody to have access to their data, 24/7, anywhere in the world. I remember one meeting where somebody said, “You know, it’s like your credit score, you can hit a button and get your score!” I asked him, “How often do you check your credit score?” Once every six or eight months, you don’t do it five times a day. I would argue if you’re checking your blood pressure every hour, then you’re a self-monitoring narcissist. Not an average human patient.
But it’s clear that patients do want access to their health system, they want engagement and co-management, they want co-production of their care.
I remember five years ago, when George Halverson [CEO of Kaiser Permanente at the time] would talk about Kaiser’s EHR, he would talk about it in Washington policy-wonk terms – how it was improving quality, how they can quickly detect side effects of new medications. Now, when I drive to the Oakland airport, I see a big sign that says, “Talk to us your way. In person, on the phone, online.”
From a patient standpoint this is less about monitoring your information, and more about electronic interaction with your healthcare system. I think within a few years if your organization can’t do that, it’s dead in the market. Once you get used to checking your lab results on your phone the day the blood was drawn, you’re never going back to, “Come in next week and we’ll talk about it.”
I turned to the ever-present question of the role of doctors in a future IT-enabled healthcare system.
MS: I’m old enough and perhaps stodgy enough to believe that, to many patients, a personal relationship with someone (often, though not always, a doctor) is an important part of the co-production of their health. That will never be replaced by a computer.
BW: Never?
MS: Yes, never.
BW: Okay.
MS: At the same time, it is neither economically sustainable nor socially necessary to have doctors doing low-value tasks. You and I both know that doctors generally overvalue the relationship with their patients – they think they are more important in their patients’ lives than their patients do. They think they spent more time with them than they did. They think they explained things to them that they didn’t. They think that their patients are more loyal to them than they actually turn out to be.
Look, all of us had to learn how to be doctors given the systems in which we worked and the technology that was available. At the time when a stethoscope was the best way to discern an S3, we learned how to use a stethoscope. That has now become not just a tool but part of our nostalgia about what it means to be a doctor. But it’s no longer the best way to figure out if a patient has a failing ventricle.
If we lament the passage of the stethoscope, and say that the iPhone is evil technology that  somehow interferes with the doctor-patient relationship, that’s just silly. It is possible for you to have your patients’ data at hand and still look that patient in the eye. You may have to rearrange your workday. You may have to rearrange your office. You may have to re-jigger the order in which you do things in your visits, but that’s adapting to new technology. At one point the stethoscope was new technology.
somehow interferes with the doctor-patient relationship, that’s just silly. It is possible for you to have your patients’ data at hand and still look that patient in the eye. You may have to rearrange your workday. You may have to rearrange your office. You may have to re-jigger the order in which you do things in your visits, but that’s adapting to new technology. At one point the stethoscope was new technology.
I am fundamentally excited by all this. Just as I am fundamentally excited by the technological advancements in drugs and devices. When I speak now, I almost always end with the story of my 71-year-old patient who has AIDS; who just had his hip replaced; who walks his grandchildren to school every day; who takes one pill once a day for his HIV. It’s a miracle.
BW: Unbelievable.
MS: I take more medicine than he does. You can’t help but be excited about what we can do for patients.
All right, so you’re going to have to incorporate these new technologies into what you do, and you’re going to have to figure out what there is that’s essential about your communication with this individual. People always resort to bemoaning the threat to the doctor-patient relationship – it’s the last refuge of scoundrels.
In my practice at San Francisco General, I’ve had the experience… I don’t know if it’s a good thing or not, but I think it’s a good thing so I’m going to keep doing it. When a patient asks me a question, I sometimes say, “You know, I don’t know the answer, let’s look it up.”
“What are your chances of developing liver cancer with hepatitis C? I want to say it’s about 14%, but I don’t know, let’s look it up.” I’ll turn the screen around and type in the search and go to a curated and reliable website, and we’ll read the answer together.
This is contrary to everything I was taught about the importance of instilling confidence in my patients by showing that I knew these things. I’m actually much more comfortable now saying, “You know, that’s a number I don’t keep in my head. And I don’t have to – let’s look it up.”
In some ways that is a marker for the issues we’re talking about. What is the essential role of the doctor, and what are roles that are better played by other people, or by technology? My forte, as a physician, is understanding what question you’re asking and trying to get you the answer, as opposed to trying to pretend that I remember all these things.


As an “older” doctor who has retired, I would like to report that I did not say “fuck it”. I said “good-bye”. There was not any anger. Only disappointment. I have nothing against quality reporting but feel the data collected that presumes to measure quality without first defining
the term is going to eventually discovered to be problematic. In the meantime, the very strength and power of the computer systems is so impressive and technologically advanced as to imply the significance of their results.
Let me tell you a story. A couple years ago, our hospital embraced a quality initiative
to measure the quality of blood glucose control in hospitalized patients. Glucose values were
recorded and quality was deemed achieved if the average blood glucose fell below a certain
number . I do not even know the number but my chart was pulled because I had a patient who had a lot of high numbers. I had to seek forgiveness for this lapse in “quality”. Perhaps
take a remedial course. Don’t remember. Seeking to clear my name I pulled the record
and found that the patient had entered in DKA with a blood glucose of around 700.
I placed the patient on an insulin drip with instructions on how to monitor and adjust the
insulin. The patient improved and the glucose readings fell 700, 633, 597, 500, 450 ,etc.
The patient stabilized and was sent home but only had 4 normal glucose readings.
I thought this was good. Treat the patient quickly, safely and discharge him. But no,
I was guilty of violating the quality requirements. You spend your life trying to help patients and wind up needing to explain to the “committee” why you failed to met their guidelines for “quality”.
I think if you look carefully at the data collected by “expert committees” like the Institute of Medicine you will find a theme running through these collections. The volume of
data has an intuitive power to overwhelm their significance. Computers are impressive.
Older doctors see this. And it is sad. We are not leaving from anger but from disappointment.
There is no turning back. We are leaving because the train is slowly and inexorably going in
the he wrong direction. By the time this is recognized and corrected we will all be gone.
Doctor, did you know the glucose level of the patient a week later? Two weeks later? That’s the benefit of standard measures and the EHR. When the patient is discharged from the hospital, he/she is still being followed by you and by others in his/her care. The outcomes will contribute to research and learning.
Really HH?
Exactly how would the data from the patient’s home glucose monitor and/or measurements and updates from other providers who interact with the patient reach the discharging hospital and other members of the patients’ care “team” (and presumably in forms that would be at all useful in following the patients’ progress)?
Ron
We’ve found that as IT becomes more prominent so to does regulatory issues and compliance. While these issues aren’t always a bad thing or prevalent, it can sometimes come as a shock to hospitals and healthcare providers just how much ‘extra baggage’ can come along with IT.