Do you have a stack of journals piling up on your desk, beside your bed or in your email inbox?
In 1950, medical knowledge was estimated to double every 50 years, but now the doubling time is every few months. At this rate, it is impossible to keep up with the literature, but a group of us worked together to boil down the top 10 articles from this past year that had practical implications for hospitalists.
Drawing from our “Updates in Hospital Medicine” presentations at Hospital Medicine 2019 and SGIM’s 2019 national meeting, Drs. Carrie Herzke, Brad Sharpe, Alfred Burger, and I worked with our colleague Anna Donovan to publish a review in Journal of Hospital Medicine of the highest impact articles and practical implications for hospitalists.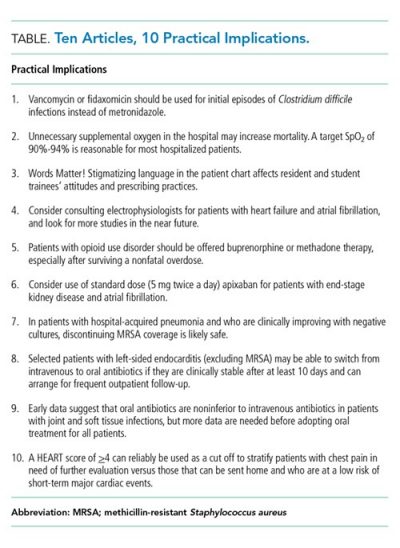
The first key practice change comes from the updated IDSA Guidelines for CDiff infection: metronidazole (flagyl) should no longer be used to treat CDiff and we should prescribe oral vancomycin or fidaxomicin, even for initial episodes and mild disease, due to improved efficacy with higher cure rates. In 2007, Professor Robert C. Reid quipped in an editorial headline that for CDiff you would want to use “Vancomycin for your mother, metronidazole for your mother-in-law.” Now the guidelines have finally caught up and the recommendation is oral Vancomycin for everyone with CDiff, even your mother-in-law!
Other highlights include clear evidence that patients with opioid use disorder should be offered treatment with either buprenorphine or methadone, especially after surviving a nonfatal overdose. According to a recent study, only 3 in 10 patients with a nonfatal opioid overdose were offered medication treatment within the following year, despite the clear mortality benefit from these medications. As the National Academy of Medicine recently loudly declared: “Medications for Opioid Use Disorder Save Lives.” Hospitalists can lead the way in ensuring that we use the “reachable moment” of hospitalization to provide patients with treatment, as described in a recent Journal of Hospital Medicine article. The other thing hospitalists can do is ensure we avoid stigmatizing language for patients with substance use disorder. A study with medical students and residents showed that the use of stigmatizing language such as “substance abuser” rather than “a person with a substance use disorder” negatively affected attitudes and prescribing behaviors. The Institute for Healthcare Improvement has started a “Recover Hope” campaign which includes a pledge to “change the narrative” related to stigma and substance use:
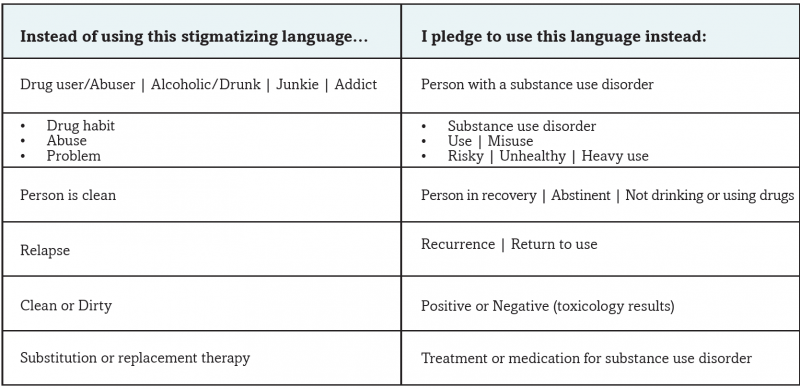
Chart from Institute for Healthcare Improvement’s “Recover Hope” campaign pledge: http://forms.ihi.org/open-school-recover-hope-campaign-change-narrative-pledge
Speaking of things we should avoid, excessive oxygen administration seems to cause harm, especially in patients with acute myocardial infarction or stroke. There even appears to be a dose-response to oxygen, with relative risk of mortality slightly rising for each percentage point INCREASE in oxygen saturation. In response, BMJ published updated recommendations, declaring that based on strong evidence we should STOP oxygen therapy no higher than 96% saturation for acutely ill adult medical patients, and we should not start oxygen therapy for patients with acute stroke or MI unless below 90-93% saturation. I know this is going to remain an uphill battle since the oxygen fairy seems to visit our patients each night and place nasal cannulas on them, without an order or anybody knowing where or when it was placed on the patient. However, our job is to take those nasal cannulas off and to start explaining to our nursing colleagues and trainees why we are doing so – we may actually be saving lives by removing supplemental oxygen!
The “POET” and “OVIVA” trials exploring early transition from IV to oral antibiotics for endocarditis and for bone and joint infections, respectively, made a big splash this year. While a number of caveats remain before widely adopting these protocols, they do suggest that many selected patients will not require 6 weeks of IV antibiotics for these conditions and can be safely transitioned to home oral antibiotics, representing a major paradigm shift.
Other key takeaways include a possible mortality benefit for ablation in patients with symptomatic atrial fibrillation and systolic heart failure, the relative safety of apixaban in patients with atrial fibrillation and end-stage renal disease, appropriate de-escalation of MRSA therapy in patients with nosocomial pneumonia, and the use of the HEART score to stratify patients with chest pain.
Check out the details, including key findings, cautions and implications for each of the articles, in our full review.



Leave A Comment